Proprioception in RCRSP Patients versus Healthy Controls

Introduction
Studies examining rotator cuff-related shoulder pain (RSCSP) often focus on prescribing exercises for (re)gaining strength and mobility. Others try to alter patient pain-cognitions and reduce kinesiophobia. Studies focusing on proprioceptive deficits are rarely published, despite already Ager et al. (2020) submitting a systematic review demonstrating proprioceptive impairments in individuals affected by shoulder pain, but further research was necessary. Proprioception is the ability to detect and sense movement and position and is an important part of the somatosensory system as it is necessary for motor control and joint stability. It is an overarching term to describe 4 different components: joint position sense (active and passive), kinesthesia, sense of force, and sense of velocity. This longitudinal study, therefore, examined shoulder proprioception in RCRSP.
Methods
This cross-sectional study was set up to compare shoulder proprioception in RCRSP patients and healthy controls. Eligible candidates with RCRSP were between 18-59 years and had the following positive clinical tests:
- Presence of a painful arc
- A positive Neer or Hawkins-Kennedy test
- A positive Jobe Test
The control participants had no history of shoulder pain or previous shoulder treatment in the last three months. They were negative on the abovementioned tests.
People with a history of shoulder surgery, or full-thickness rotator cuff tears, shoulder trauma, multidirectional instability, frozen shoulder were excluded, as well as people participating in overhead sports. Similarly, people who had current or past malign tumors, rheumatoid arthritis, cardiovascular and neurological diseases or compression syndromes of the cervical and upper arm regions were excluded from participation.
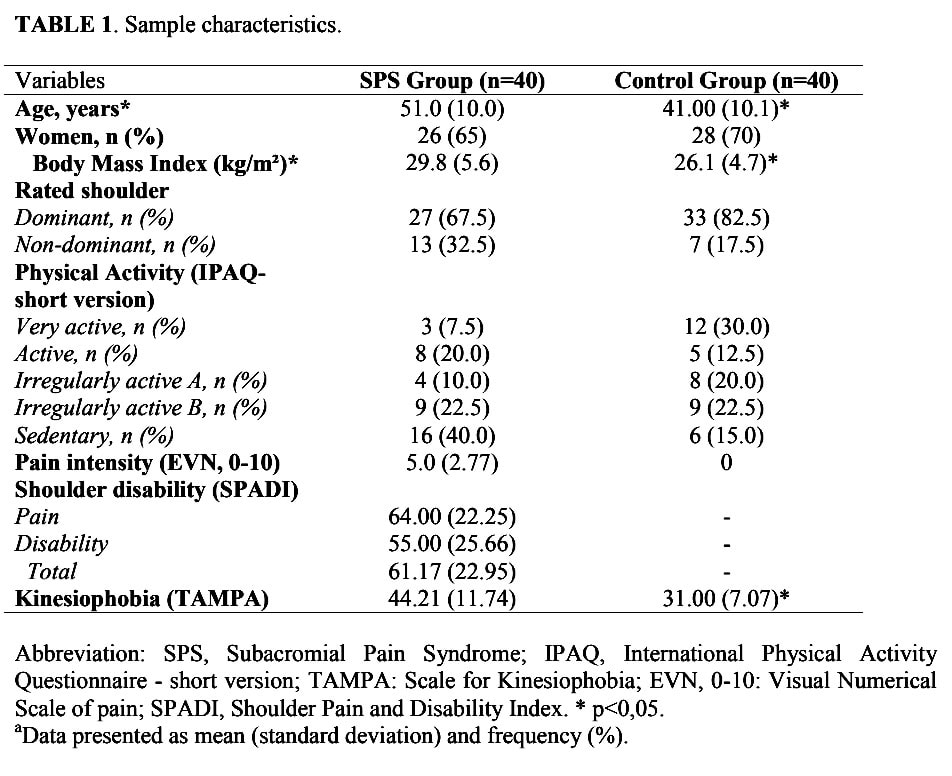
The baseline assessment included baseline demographics, anthropometrics, hand dominance and assessment of physical activity level by filling the short International Physical Activity Questionnaire (IPAQ). Participants with shoulder pain were asked to complete the Shoulder Pain and Disability Index (SPADI), the Tampa Scale for Kinesiophobia as well as the Numeric Pain Rating Scale.
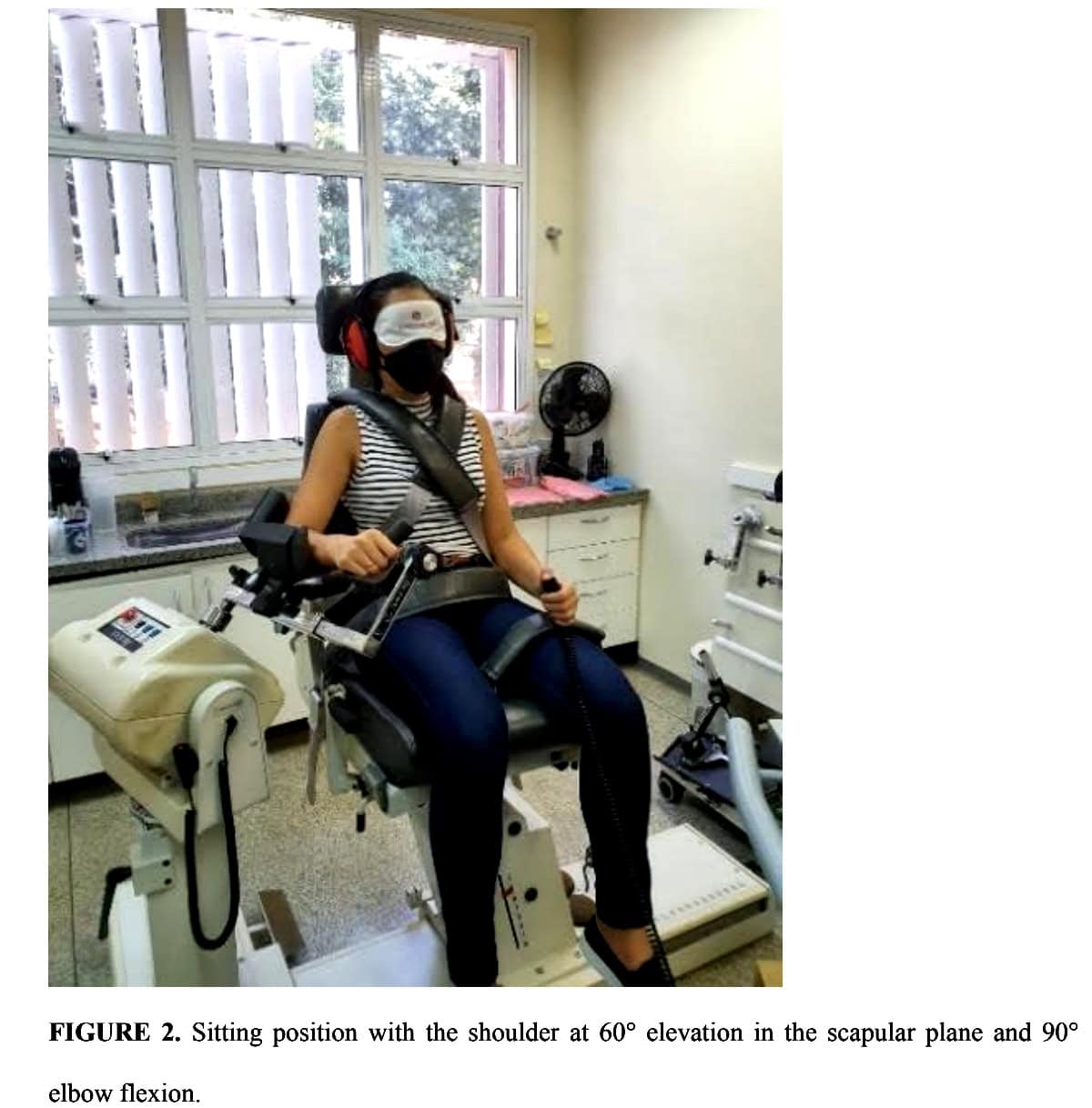
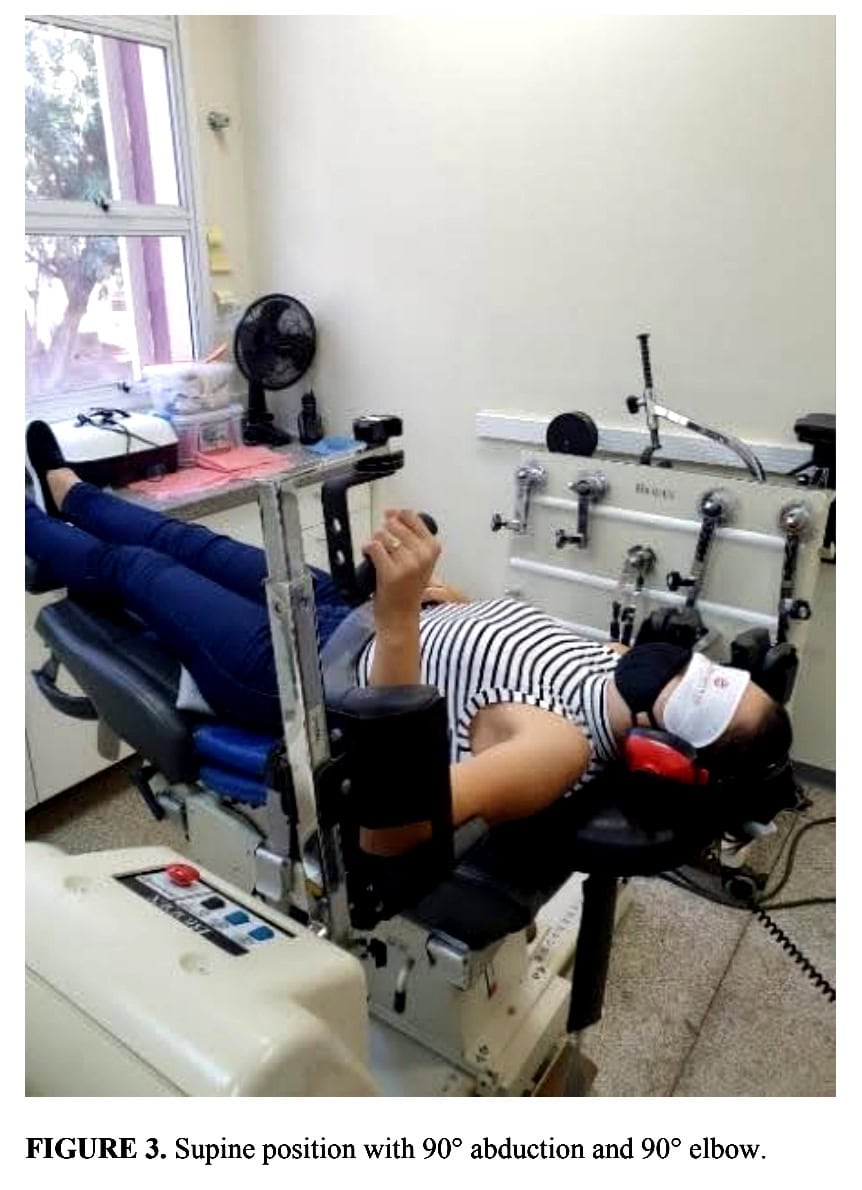
Patients with RCRSP and the healthy controls were then tested for shoulder proprioception using an isokinetic dynamometer. Two of the four components of proprioception were analyzed: kinesthesia for medial and lateral rotation, and active and passive joint position sense. Two different body positions were compared:
In the sitting position, the participants were placed with their shoulder at 60° of elevation in the scapular plane and 90° of elbow flexion.
In supine, they were positioned with their shoulder in 90° of abduction and the elbow at 90° of flexion.
Every participant completed three attempts separated by a 10-second rest interval.
Joint position sense
- Active and passive joint position sense in the seated position required the participant to sense 50° of internal and 50° of external rotation from the initial 0° position.
- During the passive joint position sense assessment the shoulder was placed in the 50° target position and held there for 10 seconds before returning to the initial position. Thereafter, their shoulder was passively moved at a 2° per second pace until the participant pressed a pushbutton when they felt they were at the target position.
- For the active joint position assessment, the same procedure was used but after the participant had the chance to feel the target position, they were asked to actively rotate their shoulder to the 50° position (at a speed of 5° per second) and press the pushbutton when they believed they reached the target.
- In the supine position, the target was 10° of medial rotation, starting from 10° lateral and vice versa. The same procedure as in the seated position was used for active and passive joint position sense.
Kinesthesia
The threshold to detect passive motion during medial and lateral rotation was assessed in seated and supine.
- In the seated position, the initial angle for lateral rotation was 0° and for medial rotation the starting position was 20° of lateral rotation.
- From the supine position, the initial angle for lateral rotation was 10° of medial rotation and vice versa.
The arm was passively moved at a 0.25°/s pace and they were instructed to push the button when they felt their arm moving. An error value was calculated by subtracting the initial angle from the final angle.
Results
Forty healthy and forty individuals with RCRSP were included. The mean age of the controls was 41 +/- 10 years and the mean age in the RCRSP group was 51 +/- 10 years. This age difference was statistically significant. Body mass index differed also statistically, with the RCRSP group having a higher BMI of 29.8 kg/m2 compared to the control group having a mean BMI of 26.1 kg/m2. The RCRSP reported a baseline SPADI score of 61.2 (+/- 23.0), indicating severe shoulder pain and functioning.
Between-group comparison
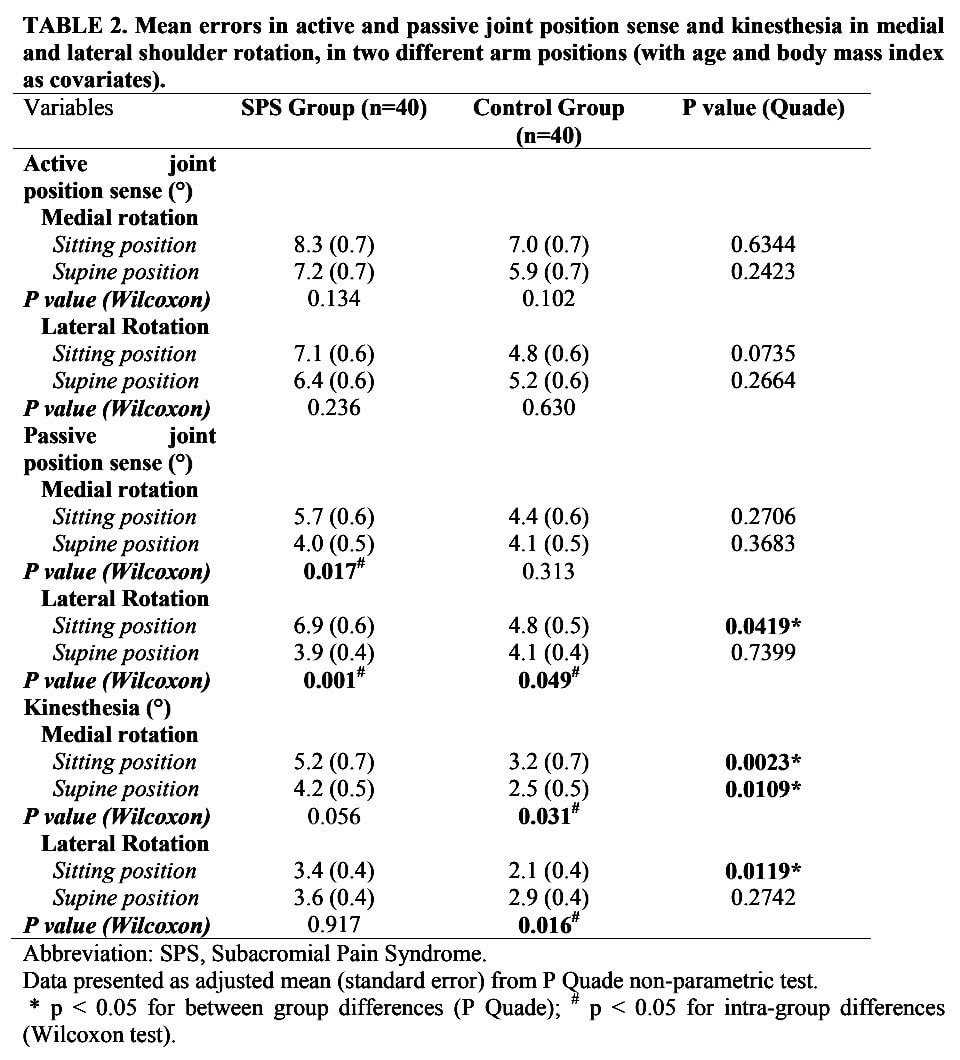
Proprioception in RCRSP patients showed significant between-group deficits in passive joint position sense for lateral rotation in sitting. The RCRSP group had higher error in the sitting position compared to the control group.
Kinesthesia showed significant between-group differences in both directions (medial and lateral) in the sitting position and medial rotation in the supine position, with the RCRSP group showing higher thresholds to detect passive motion. No differences were found between the groups for active joint position sense.
Within-group comparison
There were differences in the passive joint position sense within the RCRSP group when the sitting and supine positions were compared, both for medial and lateral rotation. In the control group only for lateral rotation, a difference appeared between the sitting and supine position.
In the control group, participants had also higher within-group errors for kinesthesia when the supine position and sitting position were compared for both medial and lateral rotation.
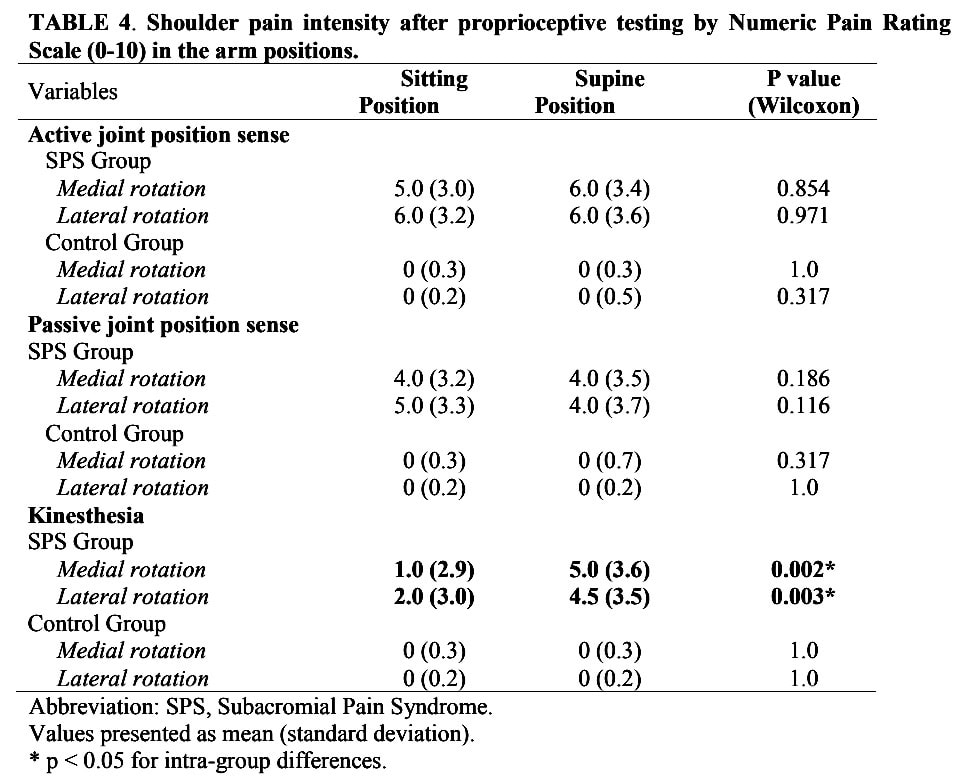
The RCRSP group reported significantly higher pain during the kinesthesia assessment in supine.
Questions and thoughts
Prior to inclusion in the study, no laxity assessment was held, for example using a Beighton score. Although the study did not use end-range positions, this was likely not necessary.
Shoulder proprioception is influenced by body position. For example, in 2003 Janwantanakul et al. demonstrated significantly poorer kinesthesia for detection of lateral shoulder rotation in sitting compared to supine lying. This is due to increased activation of shoulder structures when the joint is loaded more. In the supine position, the abduction of the arm to 90° increases stress on the articular side, bursal side, and on the M. deltoideus, independent of the load carried (Yang et al. 2023). Even in the RCRSP group, all proprioceptive measures were comparable to the control groups’ results when the participants were tested in the supine lying position, except for kinesthesia of medial rotation.
Reliability of shoulder proprioception was demonstrated to be best when assessed using an isokinetic device in 90° of shoulder abduction in the supine lying position (Ager et al. 2017). This could also explain the fact that this position yielded more accurate results. Nevertheless, the use of such a device increases the accuracy of the observed results. The use of this specialized equipment reduces the generalizability to a standard physiotherapy setting where generally no isokinetic devices are available. To incorporate proprioceptive assessment and training in your daily practice, we have a few examples to implement.
As the authors noted that people with RCRSP reported increased pain during the kinesthesia assessment in supine, you could alter the position of the patient to progress exercises aimed at improving kinesthesia. A limitation of this study lies in the assessment of pain after the test. Increased pain sensitivity during a test could potentially have decreased the proprioceptive ability. Indeed, pain sensitivity was higher in supine for kinesthesia assessment in those with RCRSP compared to sitting, yet the accuracy was not different compared to the sitting position in the RCRSP patients, while the controls had better accuracy in supine. Pain may have had a spell on this difference.
Talk nerdy to me
The authors corrected the analyses for age and body mass, since these variables were statistically different between the groups at baseline. Yet, they also report the uncorrected analyses (table 3) and describe these results in the text. This wouldn’t be necessary to do so and relying on the uncorrected analyses can give flawed results. Because the variables were non-normally distributed, the Mann-Whitney test was used to compare the two groups. This test has a null hypothesis that assumes the groups are equal, and when the null hypothesis is rejected, this means that the groups are different. The Mann-Whitney U test does not take into account covariates such as baseline differences. As a result, an observed effect may actually be a result of the initial difference and not an actual group difference. So, without correcting for baseline differences between groups, you can not rely on the statistic, and therefore, it would not have to be included in the report.
The authors also described within-group differences, accounting for differences observed between sitting and the supine position. These within-group differences are exploratory but may indicate that body position influences the accuracy of proprioceptive outcomes.
Further, no Bonferroni correction was used for the multiple comparisons, which may produce more significant results (type-1 error).
Take-home messages
Proprioception in RCRSP patients showed significant deficits in passive joint position sense for lateral rotation in sitting and kinesthesia in lateral and medial rotation in sitting and medial rotation in supine position when compared to healthy controls. As proprioception can be linked to pain, the incorporation of a proprioceptive assessment and, when appropriate, a targeted intervention, can be essential for improving RCRSP. Importantly, this cross-sectional design does not elaborate on the cause-effect relationship between RCRSP and proprioceptive deficits.
Reference
LEARN TO DISTINGUISH SHOULDER FACTS FROM FICTION
Awarded World Leading Shoulder Expert Filip Struyf takes you on a 5-Day Video Course to Bust Lots of Shoulder Myths that Prevent you From Delivering the Best Care for your patients with Shoulder Pain



