Not Meeting WHO Guidelines on Waist Circumference and Physical Activity Influences Cancer Risk

Introduction
Cancer is the second leading cause of death, behind cardiovascular disorders, and its burden grows. While genetics can play an important role, the influence of lifestyle factors is widely recognized. Healthy diets and regular physical activity have been advocated to reduce cancer risk and improve survivorship, since overweight and inactivity are important contributors to tumorigenesis. The interplay between weight and activity remains unknown. Therefore, this study looked into the relationship between those two variables and cancer risk.
Methods
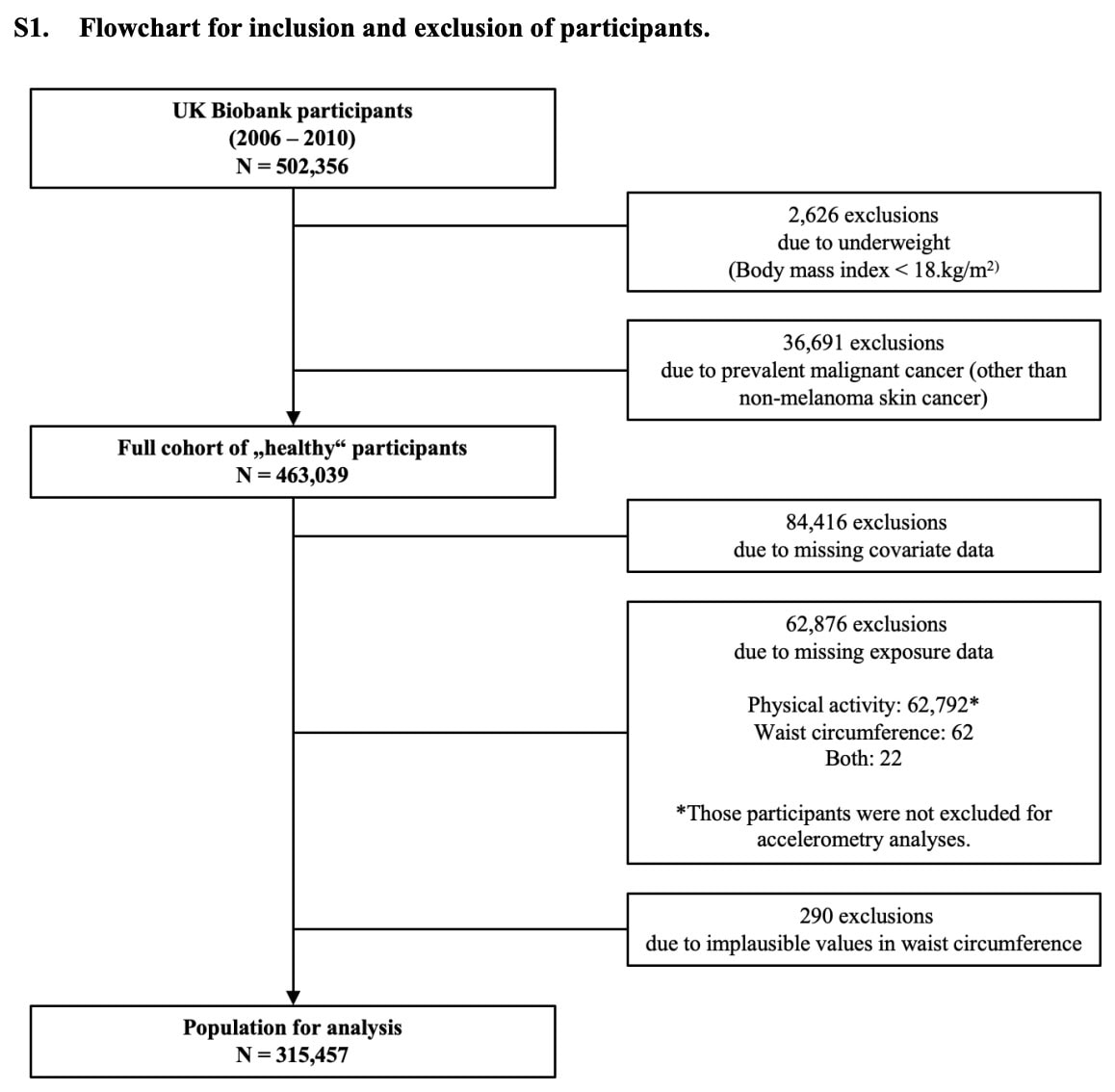
Data from the UK Biobank, a large prospective cohort that contains sociodemographic, lifestyle, and phenotypic information, was used. Individuals aged 40-69 were followed and completed physical and functional assessments, interviews, questionnaires, and delivered biological samples.
The focus of the analysis was on the relationship between waist circumference as a measure of abdominal obesity and meeting the World Health Organization (WHO) recommendations on physical activity on the risk of developing cancer in the future.
- Waist circumference was measured at the smallest part of the trunk, or at the belly button, during exhalation.
- Physical activity was measured with the short-form International Physical Activity Questionnaire (IPAQ). The IPAQ data was used to estimate the metabolic equivalents of task values (METs) according to the Ainsworth et al. compendium 2011. Moderate activities (4.0 METs) and vigorous physical activities (8.0 METs) were multiplied by their duration and frequency to calculate the MET-hours per week
A dataset of more than 315.000 people was analyzed. Participants were classified according to the WHO thresholds for abdominal obesity (waist circumference >88cm for women and >102cm for men) and sufficient levels of activity per week (>10 METs-hours/week: 4 METs x 150 minutes/60 minutes).
This classification resulted in 4 subgroups:
- Abdominal leanness and sufficient physical activity (reference group)
- Abdominal leanness and insufficient physical activity
- Abdominal obesity and sufficient physical activity
- Abdominal obesity and insufficient physical activity
The individuals in the UK Biobank were followed through the linkage with routine healthcare data and national death registries. Any cancer diagnosis was registered and used for the analyses.
Results
From the large database, 315.457 individuals were included and followed over time. Almost half of the sample were women (48.1%), and the mean age of the participants was 56.1 years at baseline.
At baseline, it was found that the group defined by abdominal leanness and sufficient physical activity had better dietary habits and lower rates of sedentary behavior and smoking, compared with the group with abdominal obesity and insufficient physical activity.
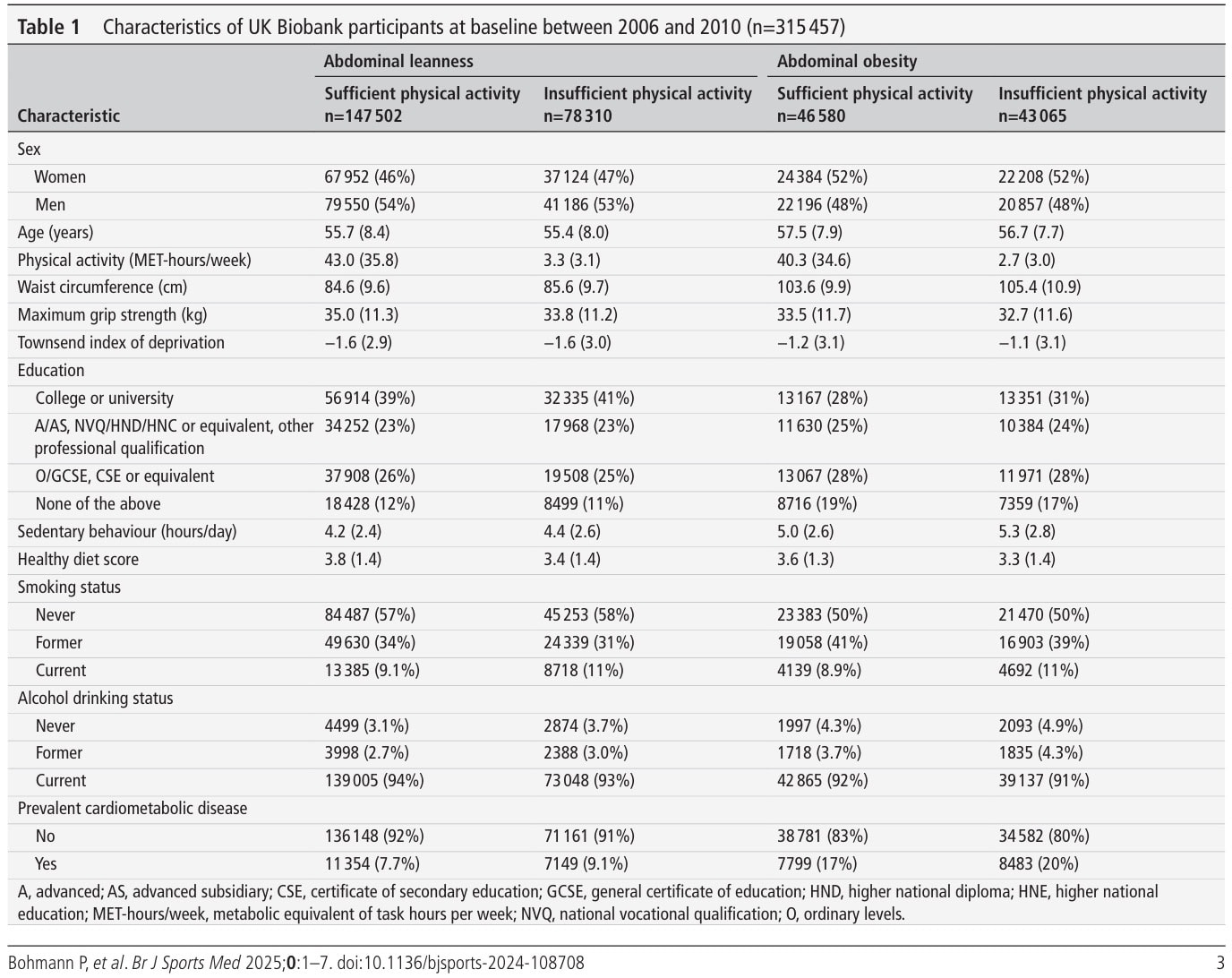
Over the follow-up period of 10.9 years, 29.710 people developed a primary malignant cancer. The group with abdominal obesity had an increased risk of developing cancer (HR= 1.11, 95%CI 1.09 to 1.14), compared with the reference group. On the other hand, insufficient levels of physical activity also heightened the risk of developing cancer (HR=1.05, 95%CI 1.02 to 1.07) compared to achieving sufficient levels of physical activity.
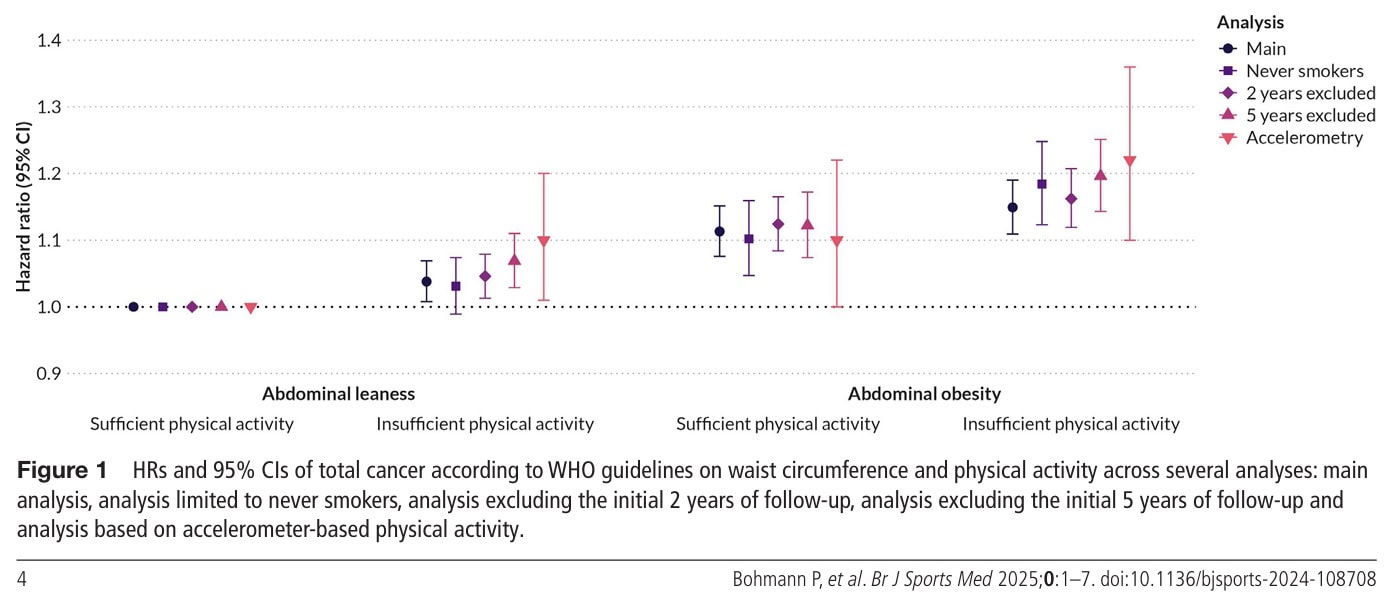
The joint associations of waist circumference and physical activity levels with total cancer risk are displayed in Table 2. Cancer risk was increased in people having abdominal obesity, regardless of their physical activity levels, although those achieving good levels of physical activity had somewhat lessened their risk (HR=1.11, 95%CI 1.08 to 1.15) compared to those with insufficient physical activity levels (HR=1.15, 95%CI 1.11 to 1.19). But abdominal leanness alone, without being physically active, is not enough, given the HR=1.04 (95%CI 1.01 to 1.07).
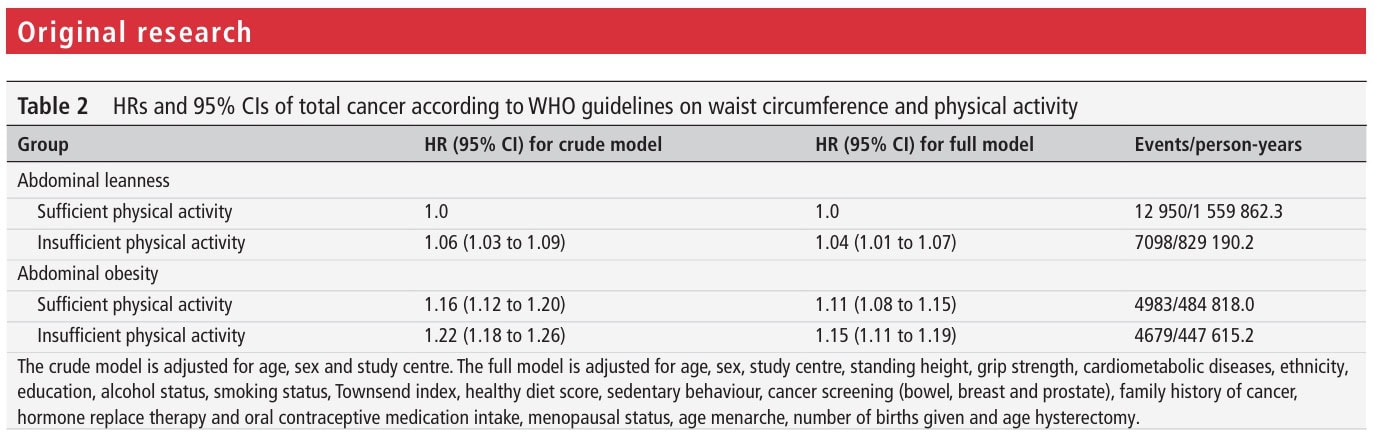
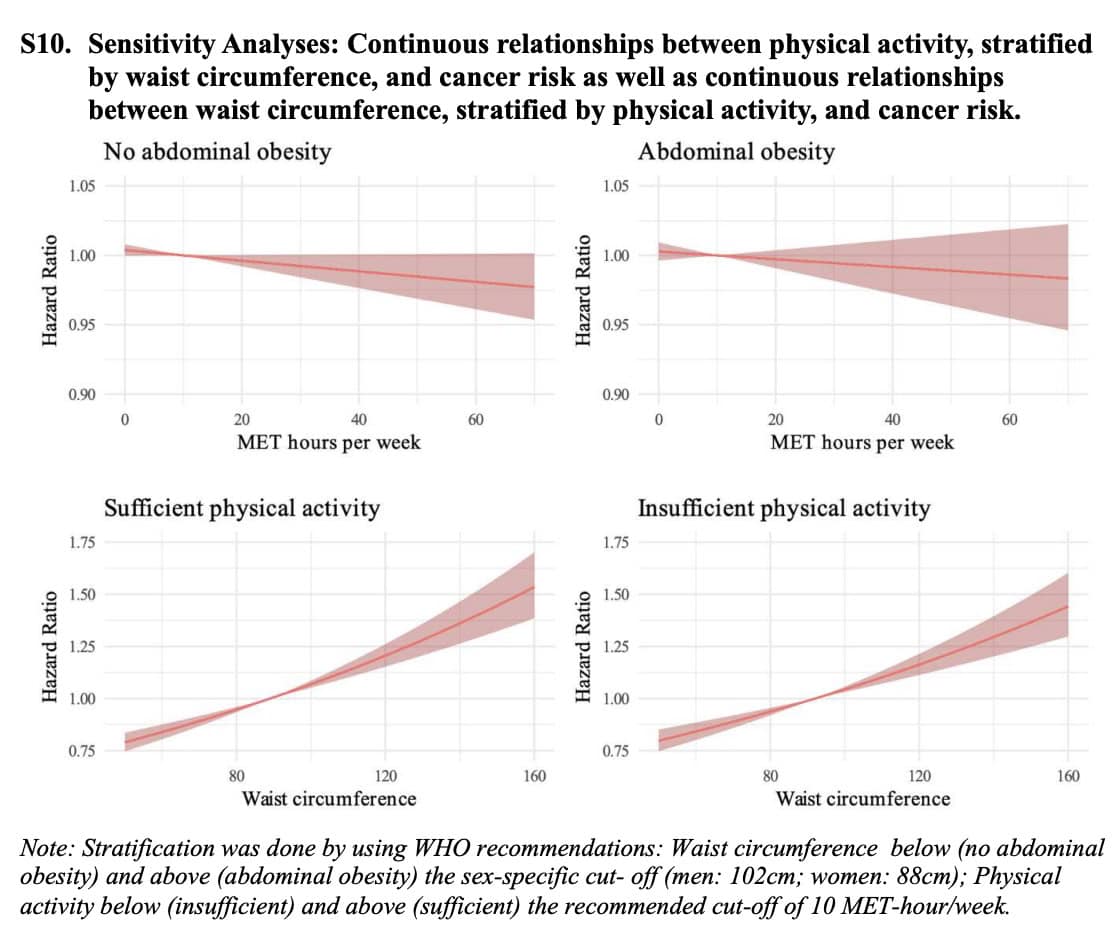
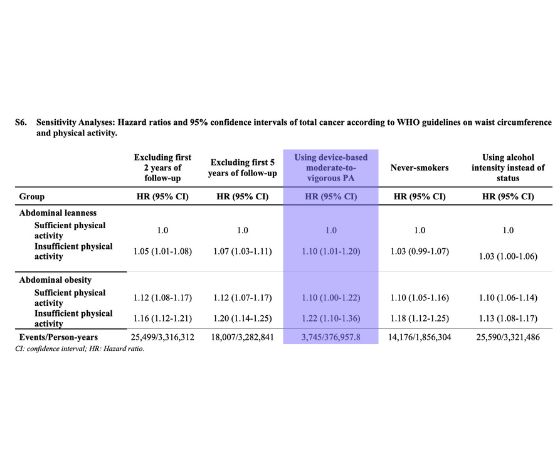
The sensitivity analyses confirmed the findings. There appeared to be no multiplication effect between waist circumference and physical activity.
Questions and thoughts
Importantly, this study did not rely on the body mass index (BMI) but on waist circumference, which is better for understanding where people’s excess body mass is distributed. High waist circumference specifically measures abdominal obesity (visceral fat), and this is linked to the occurrence of metabolic problems such as insulin resistance, inflammation, and hormonal imbalances, factors that likely contribute to cancer development. BMI can be unreliable, especially for muscled individuals, and age-related changes in body composition (an increase in fat mass and a decrease in muscle mass, despite maintaining the same weight). Somebody can lose fat mass and increase muscle mass when getting more active, but BMI can remain the same.
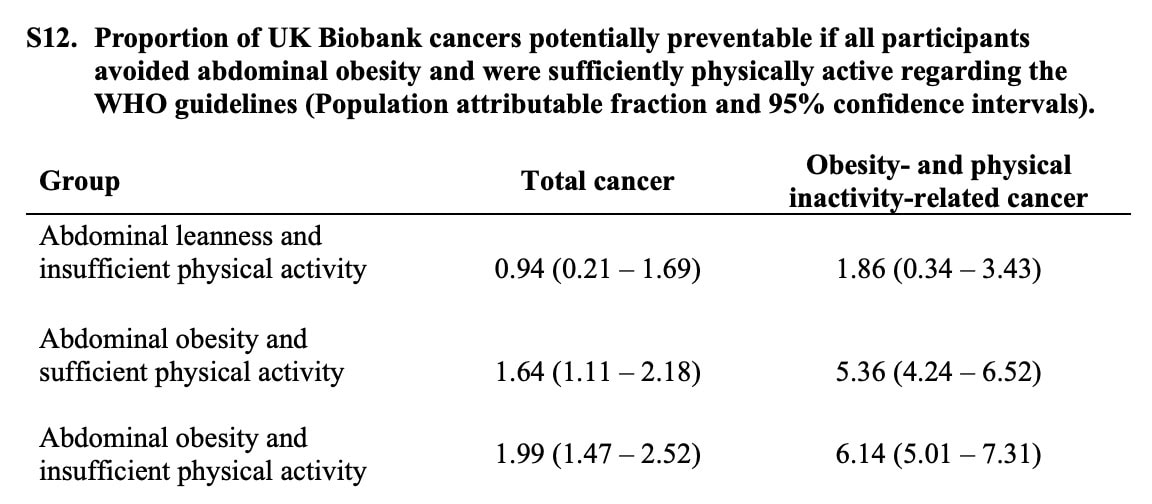
The hazard ratios revealed relevant increases in total cancer risk, but for some, it might appear small. It was estimated that abdominal obesity, coupled with insufficient activity, accounted for 2% of total cancer. However, when the authors focused on obesity- and inactivity-related cancers, the risks increased substantially. Certain types of cancer are strongly linked to being inactive and being overweight. These include esophageal (adenocarcinoma), colon, liver, endometrial, and postmenopausal breast cancer. For these specific cancers, the results were more pronounced compared to the reference group:
- Those who were abdominally obese and sufficiently active had an HR of 1.38 (95% CI 1.30 to 1.47). That is a 38% higher risk of developing obesity- and inactivity-related cancers
- Those who were abdominally obese and insufficiently active had an HR of 1.48 (95% CI 1.39 to 1.58). Meaning a 48% increased risk of obesity- and inactivity-related cancers.
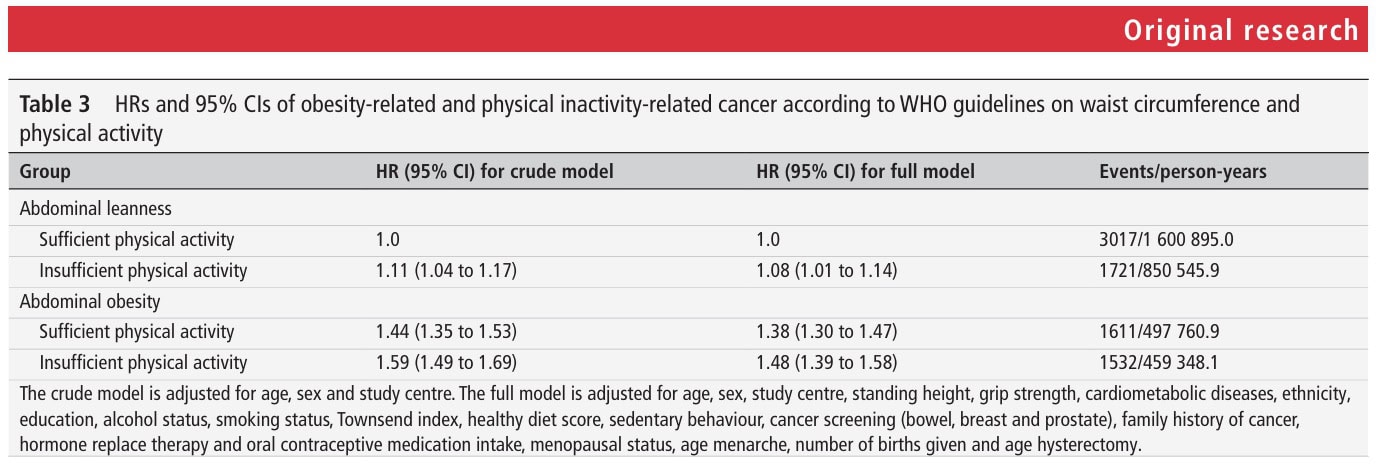
Abdominal obesity coupled with inactivity was estimated to account for 6.1% of obesity-related and inactivity-related cancers.
In the sensitivity analyses, the first 2 and 5 years of the follow-up were excluded to address the problem of reverse causation. Reverse causation means that, contrary to what you may expect, variable A is not causing variable B, but it is the other way around. In this study, the first 2 and 5 years of follow-up were excluded since the authors wanted to avoid making a false conclusion that less physical activity or increased abdominal obesity led to cancer when it was the other way around.
This is especially important since in observational studies like this one, where researchers observe associations rather than directly manipulating variables (like in a controlled experiment), there’s always a concern about reverse causation. This means that instead of the exposure (waist circumference or physical activity) causing the outcome (cancer), the outcome might actually be influencing the exposure.
For example:
- It might seem like high waist circumference causes cancer. But what if someone develops an early, undiagnosed cancer that causes them to become less active and gain weight? In this case, the cancer can be causing the high waist circumference, not the other way around.
- It might seem like low physical activity causes cancer. But what if someone starts experiencing symptoms of an undiagnosed cancer, which leads them to reduce their physical activity levels? Again, the cancer would be influencing the physical activity, not the other way around.
To address this potential issue, the researchers conducted a sensitivity analysis where they excluded participants who developed cancer within the first 2 years and then within the first 5 years of follow-up. This is important to avoid making false assumptions.
- Early Cancer Diagnoses: If someone develops cancer very soon after the study begins, it’s more likely that the cancer was already present (even if undiagnosed) at the start of the study and influencing their waist circumference or physical activity.
- Excluding Early Cases: By excluding these early cancer cases, the researchers are essentially removing individuals where reverse causation is more likely. This allows them to get a clearer picture of the potential causal relationship between waist circumference/physical activity and cancer.
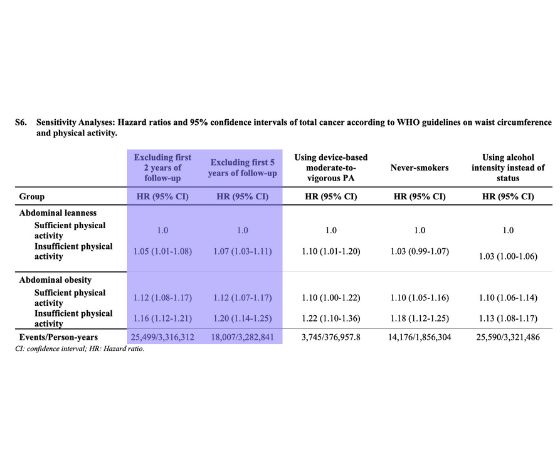
Since the study’s results remained consistent even after excluding these early cancer cases, the associations found are likely due to waist circumference and physical activity influencing cancer risk, rather than the other way around. Thus, when they took out the people who got cancer very soon after the study started (who might have already had cancer that was affecting their weight or activity), the link between waist circumference/activity and cancer was still there. This means it’s more likely that those things do affect cancer risk, and it’s not the reverse situation. This type of sensitivity analysis is a crucial step in observational studies to build confidence in the findings and address potential biases like reverse causation.
Other sensitivity analyses looked into the effect of never having smoked on the risk of people developing cancer, the amount of alcohol people consumed on the risk of cancer, the influence of accelerometer-derived physical activity levels instead of participant-reported levels of physical activity, the effect of effectively meeting the WHO’s recommended 150 minutes of moderate-to-vigorous physical activity levels per week, the influence of sex, the influence of obesity-related cancers and inactivity-related cancers, and importantly continuous rather than dichotomous physical activity levels to better define the dose-response relationships. All sensitivity analyses confirmed the primary analysis’s findings.
Talk nerdy to me
The use of such a large subset of data reinforces the findings, but as in every study, some limitations appear here as well. An important part to highlight is the measurement of waist circumference and physical activity at baseline. These variables can have changed over the years of follow-up, of course, but these changes were not taken into account in the analyses. Similarly, the UK Biobank data had a low response rate, and people who did respond were likely to have relatively high levels of physical activity (selection bias). This may mean that the real-life situation can even be worse than estimated here.
A subset of more than 72.000 people delivered 7-day accelerometer data regarding their physical activities. For the majority of people, subjective IPAQ questionnaires were used to analyze their levels of physical activity. Of course, the IPAQ-based data can be subject to recall and reporting bias, but the authors used this subjective IPAQ data and conducted sensitivity analyses using the objective accelerometer data in a subset of participants. These analyses revealed consistent results:
- The Hazard Ratio for the group with abdominal obesity and insufficient physical activity, when using accelerometer data, was HR=1.22 (95%CI 1.10 to 1.36).
- This hazard ratio was within a similar range and in the same direction as the hazard ratio obtained using the self-reported IPAQ data (HR 1.15, 95% CI 1.11 to 1.19).
Take-home messages
Not adhering to the WHO guidelines on waist circumference (>88cm for women and >102cm for men) increases the risk of cancer by 11%, and not adhering to the guidelines about physical activity (at least 150 minutes of moderate-to-vigorous physical activity per week) leads to a 5% increase in cancer risk. The combined non-adherence to waist circumference and physical activity guidelines increases the risk of developing cancer by 15%.
Regardless of genetic predisposition factors, the cancer risk can be significantly altered by maintaining a healthy weight throughout life and by engaging in regular weekly physical activity. Even if someone is meeting physical activity guidelines, having abdominal obesity still significantly increases their risk for certain cancers. This information should be used to emphasize the importance of weight management, especially reducing abdominal fat, in cancer prevention strategies for patients. We can use this information to explain to patients that even if they are physically active, having a large waist circumference still puts them at a higher risk, and addressing both factors is crucial.
Reference
How Nutrition Can Be a Crucial Factor for Central Sensitisation - Video Lecture
Watch this FREE video lecture on Nutrition & Central Sensitisation by Europe’s #1 chronic pain researcher Jo Nijs. Which food patients should avoid will probably surprise you!



