Exercise-Based Fall Prevention and Who Might Benefit From It

Introduction
Exercise-based fall prevention is widely accepted and recommended to avoid falls in the elderly population. A Cochrane review by Sherrington et al. (2020) found that exercise was able to reduce falls by 23% in community-dwelling older adults. This is especially important since falls are a major risk for rapid functional decline and decrease the survival risk significantly (Vincent et al. 2024). There are recommendations for implementing early rehabilitation after a fracture to minimize adverse effects, but preventing falls from happening can have even more impact on an individual. To effectively prescribe fall prevention exercise training, we should better understand who might benefit most from it, in order to target the right individuals effectively. However, the question of who might benefit from an exercise-based fall prevention program has not been studied extensively. Therefore, the current study questioned whether gait speed at baseline modified the effectiveness of an exercise program targeted at preventing falls in this population.
Methods
This study was a secondary analysis of a 12-month randomized controlled trial (RCT), published in 2019 by Liu-Ambrose et al., where community-dwelling participants aged 70 years and older who experienced a non-syncopal fall in the previous year were included. They were recruited from a falls prevention clinic in Vancouver, Canada.
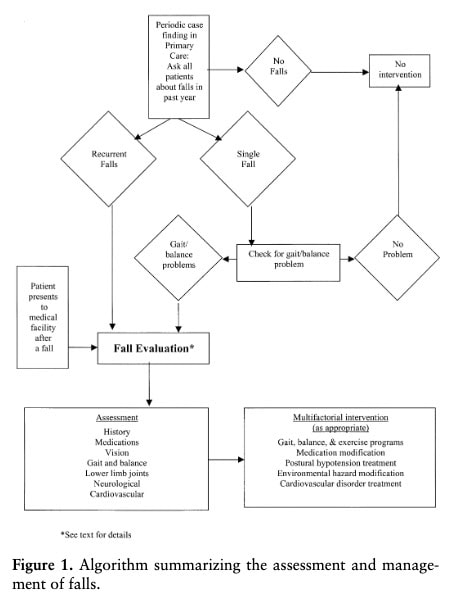
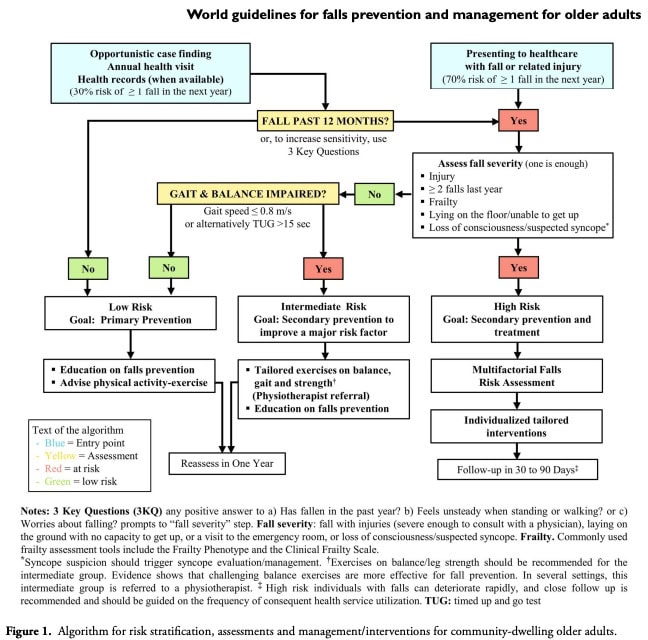
They had a fall risk assessment at the Falls Prevention Clinic, including a medical examination and treatment by a geriatrician, based on the American Geriatrics Society Fall Prevention Guidelines. This followed the following algorithm and was labeled as the standard of care pathway in this study, and could include medication adjustments, lifestyle recommendations, and referral to other health care professionals as needed.
Eligible candidates were selected based on having a higher risk of future falls based on either a Physiological Profile Assessment score of at least 1 standard deviation above age-normative values, or a Timed Up & Go Test score of more than 15 seconds, or when they had a history of 2 or more non-syncopal falls in the last year. Further, they had to have normal cognition as indicated by a score of at least 24/30 on the Mini-Mental State Examination, and a life expectancy of at least 1 year based on the geriatricians’ expert opinion. They had to be able to walk more than 3 meters.
Patients with a history of neurodegenerative diseases, dementia, stroke, or carotid sensitivity (syncopal falls) were excluded.
The original RCT randomized the participants to either the standard of care as mentioned above or to the exercise-based fall prevention program. This exercise program includes 5 strengthening exercises with progressive levels of difficulty:
- Knee extensors (4 levels)
- Knee flexors (4 levels)
- Hip abductors (4 levels)
- Ankle plantar flexors (2 levels)
- Ankle dorsiflexors (2 levels)
There were several progressive balance retraining exercises:
- Knee bends (4 levels)
- Backward walking (2 levels)
- Walking and turning around (2 levels)
- Sideways walking (2 levels)
- Toe walking (2 levels)
- Heel-toe walking backward (1 level)
- Sit-to-stand (4 levels)
These exercises were prescribed at the participants’ homes by the physiotherapist. Participants received an intervention manual describing the exercises, and cuff weights to progress the exercises in difficulty over time.
After the initial visit, the participants were asked to complete the exercises 3 times per week for about 30 minutes per session. The physiotherapist came back 3 times every 2 weeks after the initial visit to monitor the execution of the exercises and progress the exercises where possible. The final fifth visit was scheduled at 6 months. Next to performing the exercise-based fall prevention program, participants were encouraged to walk for 30 minutes, at least twice per week.
At baseline, the following measures were obtained:
- Global cognition, using the Montreal Cognitive Assessment (0-30, higher scores indicate better performance
- The Functional Comorbidity Index (0-18, higher scores indicate more comorbidities
- Independent living skills, assessed by the Lawton and Brody Instrumental Activities of Daily Living Scale (0-8, higher scores indicate more independence)
- Mood, with the 15-item Geriatric Depression Scale (0-15, scores of 5 or less represent normal mood)
- Comfortable gait speed, assessed by the 4-meter walk test, where participants began from a full stop and walked along a line indicating 4 meters. Their time was converted into speed (m/s) and categorized as slow (≤ 80 m/s) or normal (> 80 m/s), based on the World Guidelines for Falls Prevention and Management for Older Adults.
The primary outcome was the rate of self-reported falls over 12 months, captured by monthly fall calendars. Secondary outcomes measured physical and cognitive function, and included the Short Physical Performance Battery (SPPB), Timed Up & Go Test, and Digit Symbol Substitution Test (DSST).
- The SPPB measures balance and mobility and consists of a static balance test, 5 5-times sit-to-stand test, and a 4-meter walk test. Scores range from 0 to 12, and lower scores are predictive of future mobility disability.
- The Timed Up & Go Test measures functional mobility, where longer times indicate worse performance
- Cognitive functioning is measured by the DSST. Participants are presented with a legend of symbols and corresponding numbers, and they have to label a series of blank numbers with the correct corresponding symbols. Scores range from 0-84, with higher scores indicating better performance. Low performance predicts major mobility disability and subsequent falls, according to Davis et al. (2017).
The primary aim of this study was to evaluate the effects of the intervention on subsequent falls and to determine whether slow or normal gait speed influenced the effects. It was also explored whether someone’s baseline gait speed modified the effect of exercise on differences in fall rates.
Results
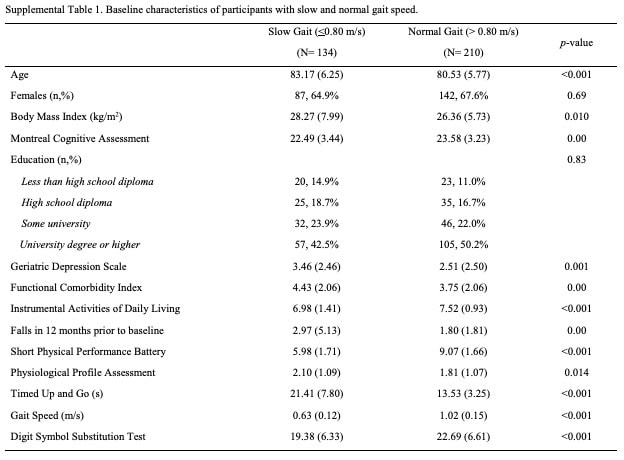
344 participants were included in this study and were equally randomized into the standard of care group or the exercise group. Their baseline characteristics are displayed below.
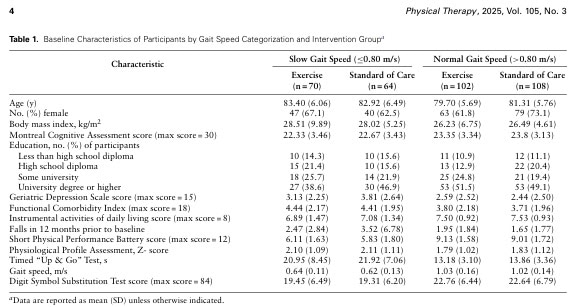
134 participants were categorized as having slow gait speed at baseline, and 210 participants had a normal baseline gait speed. There were no between-group differences in baseline characteristics among participants with slow gait speed. Participants with normal gait speed were older (mean=81.31 years; SD=5.76 years) in the standard of care group than in the exercise intervention group (mean=79.70 years; SD=5.69 years) (P =.04).
Effect on fall rates, stratified by baseline gait speed
The primary RCT found a reduced rate of subsequent falls for those randomized to the exercise-based prevention program compared with those receiving usual care provided by a geriatrician. The current analysis focused on the effect of baseline gait speed on the observed improvements in fall reduction. At 6 months, an incident rate ratio (IRR) of 0.56 was found for those with slow gait speed at baseline, compared to an IRR of 0.88 in those with normal gait speed at baseline. This means that the exercise intervention reduced fall rates significantly by 44% in those with slow gait speed at baseline. This effect disappeared at 12 months.
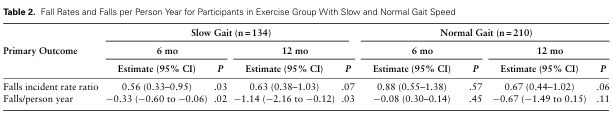
For those with normal baseline gait speed, there was no significant effect from the intervention on fall rates.
Fall rates per person year
Fall rates at 6 months in the exercise group were 0.46 falls per person year, compared to 0.79 falls per person year in the standard care group. At 12 months, this increased in both groups, to 1.81 falls per person year and 2.95 falls per person year in the exercise group and standard of care group, respectively.
When looking into this effect for baseline gait speed, fall rates in people with slow baseline gait speed showed a significant reduction in falls per person year in those randomized to the exercise-based fall prevention group, compared to those in the standard of care group at 6 months (estimated mean difference=−0.33 falls per person year; 95% CI=−0.60 to −0.06; P =.02) and 12 months (estimated mean difference=−1.14 falls per person year; 95% CI=−2.16 to −0.12; P =.03).
Among participants with normal gait speed, there were no significant differences in incident fall rates between those in the exercise intervention and standard of care groups at 6 months (IRR=0.88; 95% CI=0.55–1.38; P =.57) and 12 months (IRR=0.67; 95% CI=0.44–1.02; P =.06).
Cumulative number of falls
The standard of care group had a higher number of cumulative falls at 12 months, compared to those in the exercise group. This difference was regardless of the baseline gait speed status. Surprisingly, those with slow gait speed at baseline randomized to the exercise group had the lowest number of cumulative falls at 12 months.
The exploratory secondary outcomes were in line with the observed improvements in the primary analyses:
- Timed Up & Go Test scores became faster in the exercise group at 6 months, indicating faster walking pace
- At 12 months, the exercise intervention group had better DSST performance, indicative of improved cognitive processing speed
- No differences were observed after completing the intervention in the group with normal baseline gait speed
Questions and thoughts
These participants were recruited from a specialized care setting, which may have important implications for routine physiotherapy practice. They had been seen by a geriatricist and screened for medical conditions, medication, vision, neurological functioning, mental status, cardiovascular, and autonomic functions. Be aware that you should check these items in a patient presenting to you who has not seen a specialist before seeing you. Ideally, aim to establish a close collaboration with the patient’s general practitioner, as older individuals who are at risk of falling can be better managed on a multidisciplinary level.
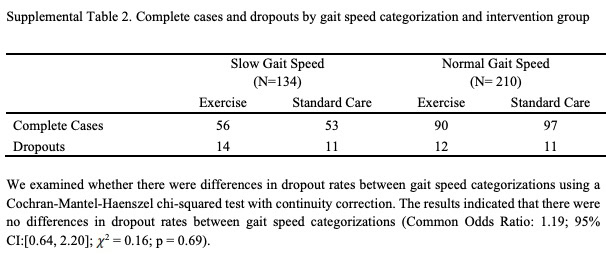
There appeared to be no differences in adherence to the exercise-based fall prevention intervention between slow-paced and normal-paced individuals. The authors, therefore, concluded that the intervention was feasible for both the slow-paced and normal-paced individuals. Of note, however, is that the adherence was reported to be around 50%, meaning that only half of the prescribed sessions were completed, on average. Knowing that only 12 sessions per month were required (3 sessions per week), the observed benefits can potentially be increased with better supervision and guidance.
We should also be aware that the individuals reported their adherence to the exercise-based fall prevention program by mailing monthly calendars or by telephone calls. Desirability bias may arise here, where respondents tend to answer questions in a manner that will be viewed favorably by others. They may over-report adherence to the exercise sessions, for example. Of course, recall bias may also have played a role, especially when looking back on their adherence for a whole month. Ways to improve adherence to effectively stimulate participants to complete the fall prevention program should be prioritized, as there may be great room for improvement of the observed effects.
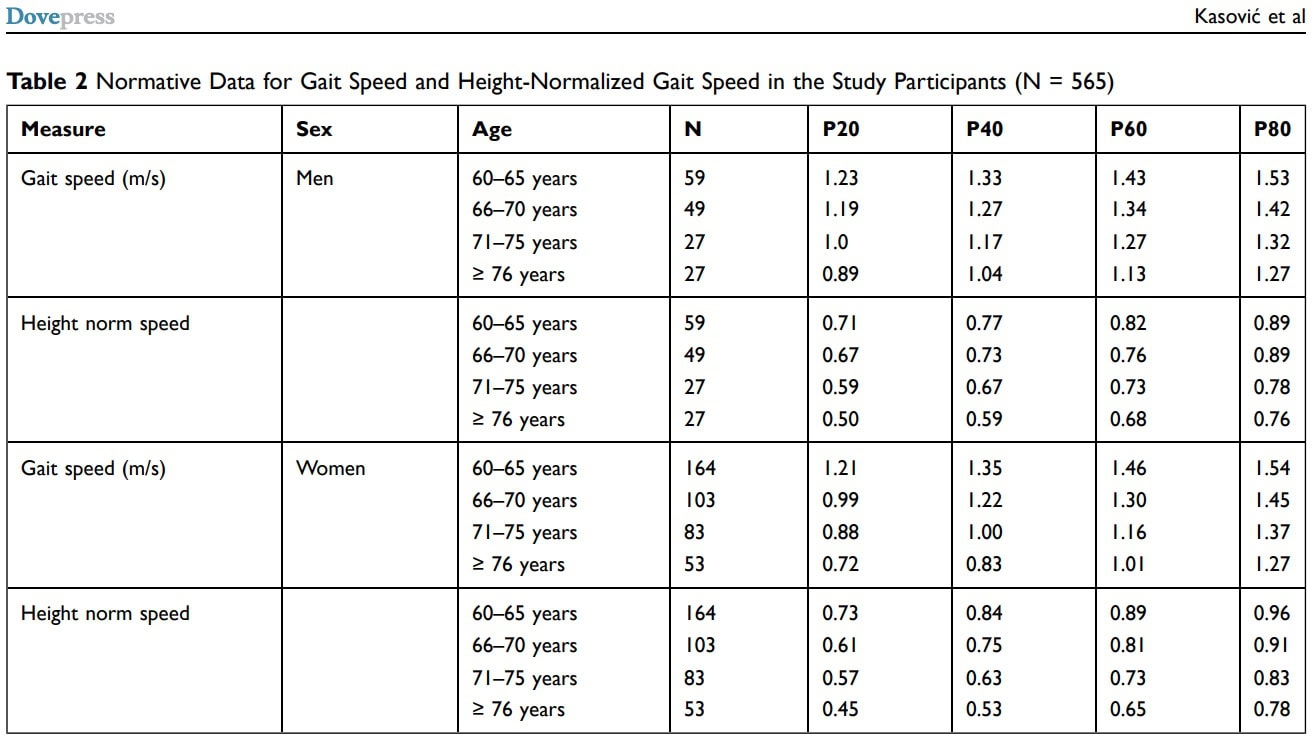
A limitation of this study was that the categorization of gait speed into slow and normal was not based on age-matched normative values, but based on a fixed cut-off of 0.80 m/s. Older adults will show a decline in speed, but when comparing everyone for the same threshold, this may have led to miscategorizations. Although this cut-off was based on the recommendations of the World Guidelines for Falls Prevention and Management for Older Adults, this is something to consider. Kasović et al. (2021) established normative values per age category in older adults and found that only a minority of their sample had gait speeds below 0.80 m/s. Indeed, they potentially recruited more fit participants, as they were recruited from the Society for Sport Recreation for older people in the city of Zagreb, but the normative values show that categorizing someone of 70+ with a gait speed of around 0.9 is not necessarily a fast-paced walker, as their norms also show paces of around 1.0 plus. The use of the 0.80 m/s threshold can be an important indicator of increased fall risk, but compare the individual to their normative reference group and aim to reach higher in rehab than the recommended cut-off of 0.80 m/s as used here for analysis purposes.
Talk nerdy to me
Randomization was stratified by sex since fall rates differ between males and females, but sex was not taken into account for the gait speed measurements. I would suggest using normative values to compare a patient on the level of the individual, instead of on a group level.
Significant baseline differences emerged: the normal gait speed group was on average younger, better in physical performance scores (SPPB and Timed Up & Go), and had better cognitive function, fewer comorbidities, and better independence. While the secondary outcomes were corrected for these baseline differences, the primary analysis was not. This means that any pre-existing differences in these characteristics could have potentially influenced the observed differences in fall rates between groups. Therefore, this accounts for a huge limitation of this study. While the study highlights significant fall reduction in the slow gait speed group at 6 months, it’s still possible that some of this effect could be related to the baseline differences between groups, not just the intervention. But the secondary analyses did include baseline differences in the linear mixed models as covariates and supported the findings of the primary analysis, adding another layer of understanding to the findings.
No differences in dropout rates appeared between participants with slow and normal gait speed, indicating the feasibility of the exercise-based fall prevention program.
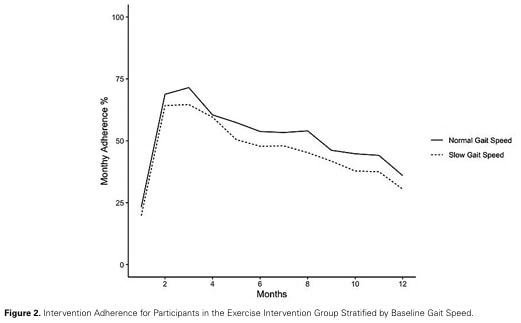
The question arises whether better adherence could improve the observed risk reductions even further. If so, more close monitoring and guidance should be recommended, especially for those with already slow gait speeds. Likewise, older people with slow gait speeds who have not yet fallen should be counseled on falls prevention and should be advised to participate in physical activities and exercise (primary prevention). Also, the disappearing risk reduction at 12 months may indicate that a continuing, ongoing intervention would be appropriate to maintain the significant improvement in reduced fall risk.
As this study was a secondary analysis, it was not adequately powered for its research questions. The outcomes observed here should now be tested more rigorously in a primary analysis RCT. There was no correction for multiple outcomes, which is something that should be incorporated into future studies.
Take-home messages
Exercise-based fall prevention can reduce fall risk significantly. Baseline gait speed was shown to be a significant modifier of the effectiveness of this intervention program. This indicates that older individuals who have already experienced a fall benefit more from such an exercise intervention when they have a slow gait speed (≤ 0.80 m/s) in the short term (6 months). The effect disappeared at 12 months, indicating that a continuing intervention might be needed. Exploratory secondary analyses indicate that the reduction in fall risk goes along with improvements in functional mobility (Timed Up & Go) and cognitive function (DSST) in those with slow baseline gait speed. Older adults who have fallen and who have slow gait speeds should have access to exercise-based fall prevention interventions and should be prioritized to reduce the risk of subsequent falls and related decline in their health status.
Reference
100% FREE POSTER PACKAGE
Receive 6 High-Resolution Posters summarising important topics in sports recovery to display in your clinic/gym



